Reimagining the Scalpel: 3D Printing as Disruptive Innovation for Global Surgery
- nicholaschapmannz
- Apr 24, 2025
- 2 min read
Updated: May 1, 2025
In global surgery, we talk a lot about training, capacity-building, and partnerships. But one of the most fundamental—and overlooked—barriers remains the surgical supply chain. Who makes the tools? Who delivers them? And who decides what gets where, when? As the call to “decolonize global health” intensifies, we must ask: are we simply repackaging colonial dynamics in modern terms?
We must decolonize the decolonization movement itself, as rhetoric alone won’t disrupt entrenched hierarchies [1]. Real power lies in self-reliance. That’s where technology steps in.
Operating rooms are among the most environmentally harmful spaces in any hospital, consuming up to six times more energy than other spaces and producing significant waste [2]. Now add to that the carbon cost of shipping thousands of tons of surgical supplies across the globe. The environmental and ethical costs stack up fast.
But what if we flipped the model? What if low-resource hospitals could manufacture their own surgical instruments—scalpel holders, retractors, clamps—on site?
Disruptive innovation isn’t just for Silicon Valley. As Christensen and colleagues argued, the most powerful innovations are those that redefine how services are delivered to underserved communities [3]. 3D printing surgical tools in hospitals like Chris Hani Baragwanath Academic Hospital in Johannesburg is not just feasible—it’s already happening. I brought a 3D printer to Uganda, and the first print was a working scalpel holder. Proof of concept. And yes, filament can be delivered even to rural areas.
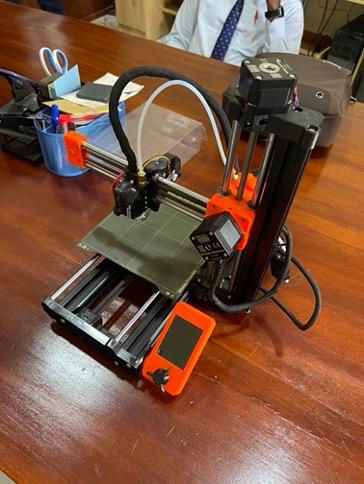
![3D-printed scalpel handles composed of polylactic acid filament, a renewable and biodegradable bioplastic made from fermented plant starches. Using PLA, these scalpel handles can be produced for about $1 USD per unit, and while they are not compatible with autoclaving, they can be safely sterilised [4], and future iterations printed with other materials such as carbon fibre will be autoclave-compatible.](https://static.wixstatic.com/media/d7b31e_b2cf6c987e1e4a55b2e278b623a8a648~mv2.jpeg/v1/fill/w_686,h_684,al_c,q_85,enc_avif,quality_auto/d7b31e_b2cf6c987e1e4a55b2e278b623a8a648~mv2.jpeg)
This is about more than cost-cutting. It’s about climate responsibility, self-determination, and local resilience.
To show just how possible it really is to harness cutting-edge technology to create solutions that feel magical, consider this:
This entire post was written using artificial intelligence, without a single word typed by the author. Just themes, ideas, and articles shared by the author with ChatGPT through dictation.
The future is already here.

Dr Saad Sahi is a General Surgeon and Acute Care Surgery Fellow at Brigham and Women's Hospital, the teaching hospital for Harvard Medical School. He has a keen interest in developing innovative and scalable solutions for surgical education and infrastructure, particularly in underserved areas, and has spent several years working in rural Uganda and the Navajo nation.
References
[1] Bua E, Sahi SL (2022). Decolonizing the Decolonization Movement in Global Health: A Perspective from Global Surgery. Frontiers in Education. Available from: https://www.frontiersin.org/articles/10.3389/feduc.2022.1033797/full
[2] Hey MT, Shoyombo I, Yates EF, Anderson GA. (2022). Climate Change and Global Surgery. Think Global Health. Available from: https://www.thinkglobalhealth.org/article/climate-change-and-global-surgery
[3] Christensen CM, Baumann H, Ruggles R, Sadtler TM (2006). Disruptive Innovation for Social Change. Harvard Business Review. Available from: https://hbr.org/2006/12/disruptive-innovation-for-social-change
[4] Pérez-Davila S, González-Rodríguez L, Lama R, et al (2022). 3D-Printed PLA Medical Devices: Physicochemical Changes and Biological Response After Sterilisation Treatments. Polymers. 14(19):4117.
